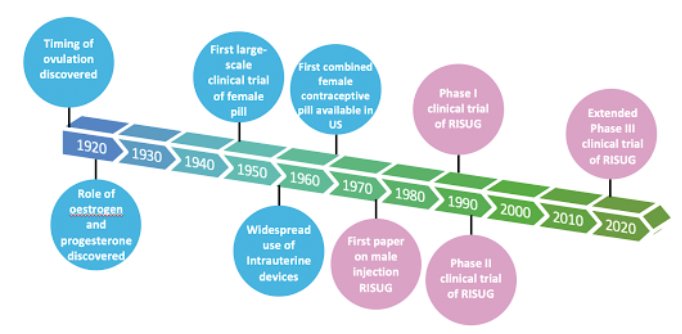
Conversely, female birth control methods, such as oral contraceptive pills and intrauterine devices (IUDs), have long since dominated the market due to a combination of cultural, religious, and socioeconomic factors.
Research has come a long way since Ancient Egyptians used honey and lemon as a spermicide in 3500 BC, with a whopping 257 female contraceptive pills available on the market today. In stark comparison to major growth in the female contraceptive industry over the past century, the stagnation of the male contraceptive pill market is rather surprising.
When developing the ideal contraceptive, there are several boxes to tick:
Easy to use and rapidly effective
Favourable safety and tolerability profiles
Reversible
Acceptable to both partners and does not affect libido
Inexpensive and readily available
Hundreds of female contraceptive drugs have managed to pass this checklist, yet the situation is quite the opposite for male contraceptive alternatives despite our modern-day scientific knowledge of the male reproductive system. To understand the position of the male contraceptive industry, scientific research, public opinion, global potential and cost effectiveness must all be considered.
There are four categories of male contraceptive methods undergoing clinical trials: male birth control pills, male contraceptive gels, nonhormonal options and vas-occlusive contraception.
Male birth control pills work similarly to their female counterparts in that they both target molecular receptors to manipulate hormonal activity. Dimethandrolone Undecanoate (DMAU) and 11β-Methyl Nortestosterone (11β-MNT) both bind to androgen and progesterone receptors. Daily oral DMAU, Injectable DMAU and 11β-MNT are currently under evaluation in Phase I clinical trials.
The daily male contraceptive Nestorone (NES) and Testosterone (T) (NES/T) combination gel works quite differently. The gel is applied to the shoulders and upper arms for 4 hours every day and reduces sperm concentration from the normal level of < 15 million/mL to < 1 million/mL.
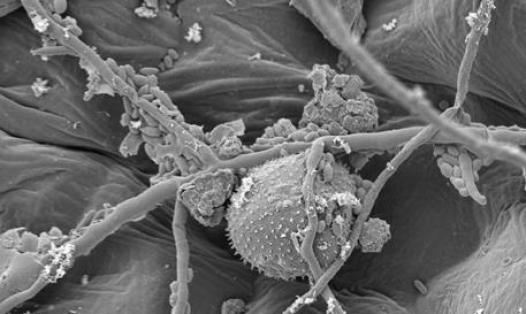
Nonhormonal drugs target genes and proteins essential for male fertility. One such example is a soluble adenylyl cyclase (sAC) inhibitor that inhibits a molecule called ADCY10 found only in male germ cells. Another nonhormonal male contraceptive target is the Epididymal Protease Inhibitor (Eppin), which binds to a protein in the semen called semenogelin. Developing a small organic compound that binds to Eppin and mimics the effects of semenogelin would result in a rapid decrease in sperm intracellular pH and calcium levels, and ultimately prevent sperm motility.
Vas-occlusive contraception blocks sperm transport in the vas deferens. The front-runner in the male contraceptive alternative industry, RISUG (Reversible Inhibition of Sperm Under Guidance), falls under this category. RISUG is a gel-based polymer which coats the inner walls of the vas deferens (the tube that carries sperm to the urethra) and affects sperm mobility, whilst still allowing fluid to pass through.