
The determinants of pericyte tone are poorly understood. We show that a small rise in cytoplasmic Ca2+ concentration ([Ca2+]i) in pericytes activates chloride efflux through the Ca2+-gated anion channel TMEM16A, thus depolarizing the cell and opening voltage-gated calcium channels. This mechanism strongly amplifies the pericyte [Ca2+]i rise and capillary constriction evoked by contractile agonists and ischemia.
In a rodent stroke model, TMEM16A inhibition slows the ischemia-evoked pericyte [Ca2+]i rise, capillary constriction and pericyte death, reduces neutrophil stalling and improves cerebrovascular reperfusion. Genetic analysis implicates altered TMEM16A expression in poor patient recovery from ischemic stroke. Thus, pericyte TMEM16A is a crucial regulator of cerebral capillary function, and a potential therapeutic target for stroke and possibly other disorders of impaired microvascular flow, such as Alzheimer’s disease and vascular dementia.
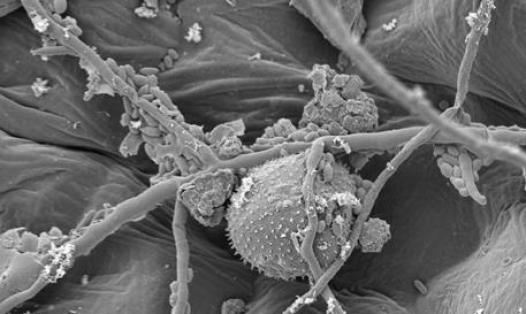
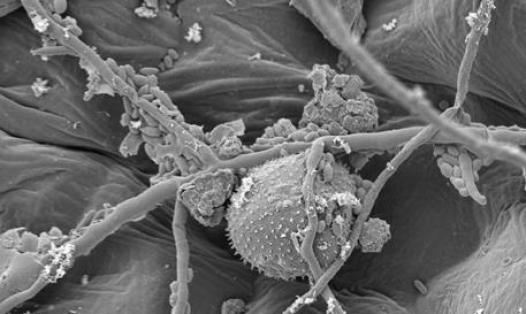
Cerebral blood flow (CBF) is regulated both at the arteriole and at the capillary level (1, 2), indeed capillaries are the site of highest vascular resistance within the brain parenchyma where neuronal activity can influence vessel diameter (3, 4). Capillary resistance can be altered by changes in the tone of contractile pericytes with processes running circumferentially around the capillaries (5, 6).
Electrical stimulation, optogenetically-induced depolarisation, contractile agonist application and optical ablation of single cortical pericytes have demonstrated the capacity of pericytes throughout the capillary bed to contract and control capillary diameter and local blood flow (7-13).
Alterations in pericyte contraction are crucial in the pathogenesis of ischemic stroke (6), Alzheimer’s disease (11), spreading depolarisation (e.g. during migraine with aura) (12) and neurological problems following cardiac arrest (13). After ischemic stroke, when blood flow to the occluded artery is restored, capillaries remain under-perfused (14, 15) even when thrombolysis is initiated shortly after stroke onset (16). This “no-reflow phenomenon” impairs patient recovery (17).
The lack of reflow is largely due to pericytes constricting capillaries during and after ischemia (6, 18), possibly as a result of the cytoplasmic Ca2+ concentration ([Ca2+]i) rising in pericytes after a fall of ATP level ([ATP]i) inhibits ion pumping, although release of vasoconstrictors, such as endothelin-1 (ET-1) and thromboxane, in ischemic stroke may also contribute (19-21).