Across all, there is now a clear emphasis on the need to incorporate a One Health approach, recognizing the critical links between human and animal health and the environment. Schistosomiasis, caused by Schistosoma spp. trematodes, is a NTD of global medical and veterinary importance, with over 220 million people and untold millions of livestock currently infected. Its burden remains extremely high in certain regions, particularly within sub-Saharan Africa, despite over two decades of mass preventive chemotherapy (mass drug administration), predominantly to school-aged children. In Africa, in contrast to Asia, any zoonotic component of schistosomiasis transmission and its implications for disease control has, until recently, been largely ignored. Here, we review recent epidemiological, clinical, molecular, and modelling work across both Asia and Africa. We outline the evolutionary history and transmission dynamics of Schistosoma species, and emphasize the emerging risk raised by both wildlife reservoirs and viable hybridization between human and animal schistosomes. To achieve the 2030 WHO roadmap elimination targets, a truly multi-disciplinary One Health perspective must be implemented.
This article is part of the theme issue ‘Challenges and opportunities in the fight against neglected tropical diseases: a decade from the London Declaration on NTDs’.
Momentum in the fight against neglected tropical diseases (NTDs), 20 epidemiologically complex conditions that predominantly affect impoverished communities [1], has been building alongside a change in targets from morbidity control to elimination. With renewed emphasis on the need to incorporate a One Health approach, ‘an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals and ecosystems' [2, p. viii], the World Health Organization (WHO) has launched a series of documents over the past 3 years, including a revised 2021–2030 NTDs roadmap [3], a revised Guideline on control and elimination of human schistosomiasis [4], a companion One Health approach document for action against NTDs [2], a global strategy on water, sanitation and hygiene (WASH) to combat NTDs [5], and a 2022–2026 One Health joint plan of action in conjunction with other international agencies [6]. These documents serve to embed One Health at the heart of control efforts for NTDs with significant environmental or zoonotic epidemiological characteristics and stress the importance of One Health in sustainably improving the intertwined health of humans, animals and their ecosystems [2].
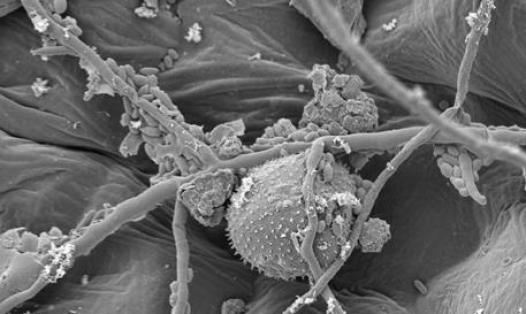
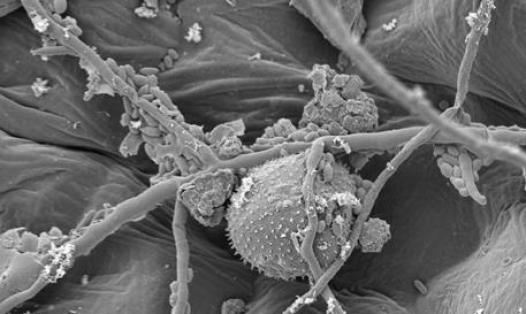
Schistosomiasis is among the most important NTDs and is estimated to infect a quarter of a billion people worldwide [7,8]. This debilitating parasitic disease is present in 78 tropical and subtropical countries, with major foci across Asia, Africa and South America [3], and a potentially emerging focus in southern Europe [9]. However, its burden is placed overwhelmingly on sub-Saharan Africa (SSA), where 90% of human schistosome infections occur [7,10,11], causing approximately 24 000 deaths and at least 2.5 million disability-adjusted life years (DALYs) [3]. The parasite's environmental infective stages—snail-infective miracidia and mammal-infective cercariae—are restricted to freshwater habitats of the snail intermediate host, thus schistosomiasis is considered a water-borne disease [5], with ongoing debates for and against its classification as a vector-borne disease [12,13]. Importantly, the clinical consequences of infection by schistosomes are experienced not only by humans, but also by non-human mammalian definitive hosts [14], many of which can act as reservoirs of subsequent human infection for certain schistosome species [15–17].
As of January 2020, of 78 endemic countries 51 are targeted for mass preventive chemotherapy (i.e. mass drug administration, MDA, using praziquantel) by WHO owing to moderate to high schistosome transmission [3]. The 2030 WHO schistosomiasis elimination goals call for its elimination as a public health problem (EPHP) from all endemic countries—42 in Africa, ten in the Americas, three in Southeast Asia, six in the western Pacific, 16 in the eastern Mediterranean and one in Europe [18]—with EPHP defined as less than 1% heavy-intensity infections (≥50 eggs per 10 ml urine or ≥400 eggs per gram of stool are indicative of a heavy-intensity infection [18]). After 20 years of large-scale MDA, morbidity profiles have shifted; thus a revised EPHP definition based on overall infection prevalence instead of heavy-intensity infections has recently been advocated [19]. In addition to EPHP, interruption of transmission (IoT) in 25 of the 78 endemic countries has also been set as a WHO schistosomiasis elimination goal, with IoT defined as absence of infection in humans [3]. WHO's EPHP goal has been met in China since 2015 [20] but further national control efforts aim for transmission control as well as transmission interruption. Transmission control is defined by Chinese authorities as less than 1% infection prevalence in humans and livestock, plus two consecutive days of negative malacological surveys and no acute schistosomiasis cases [20]—although schistosomiasis is most commonly a chronic disease, an acute presentation has been described in humans [10] and livestock [21]. Transmission interruption is defined by Chinese authorities as absence of infection in humans, livestock and snails for five consecutive years [20].
The WHO roadmap [3] identifies a number of actions required to reach the schistosomiasis elimination targets, which include: more comprehensive MDA strategies (e.g. expanding to include more demographic groups, ensuring access to therapeutics, developing alternatives to praziquantel); snail control (e.g. developing appropriate guidelines for targeted snail control and alternative control methods); improved diagnostics—for humans and animals—for micro-mapping; and the creation of cross-sectoral mechanisms to coordinate key sectors like WASH, environmental management and animal health. The roadmap also expounds on the risk posed by zoonotic reservoirs in Asia and beyond, advocating wider use of veterinary public health interventions [3]. Specific points for consideration include improved sanitation and management of animal waste, keeping animals away from transmission sites and treating animals with praziquantel. The companion One Health approach WHO document [2, p. xi] ‘provides guidance on the One Health actions needed by major stakeholders and how to support a paradigm shift towards One Health in national NTD programmes', and is complemented by the One Health joint plan of action [6] framework to support and expand One Health capacities at global, regional, and national level. Hence, the One Health approach is now firmly embedded within WHO guidance on eliminating schistosomiasis.
Operationalizing One Health measures for zoonotic NTDs is nevertheless challenging (see [22]). For instance, despite long-standing knowledge of the effectiveness of anti-rabies dog vaccination in preventing human deaths [23], capacity building for mass dog vaccination is still a critical action required to reach the 2030 rabies elimination targets [3]. Moreover, the recent detection of Dracunculus medinensis infections in animals [24] has triggered a focus on emerging animal reservoirs to reach dracunculiasis eradication targets [3]. Indeed, there are now more infections recorded in non-human mammals (mostly domestic dogs, some domestic cats and a few baboons [25]) than in humans [24]. Interestingly, a non-classical transmission pathway in dogs likely contributing to disease persistence has been identified in Chad [25].
In this perspective, we first consider recent advancements in understanding the evolutionary history and transmission dynamics of Schistosoma spp., before outlining the emerging risk posed by wildlife and livestock reservoirs of infection and hybridization between human-infective and livestock-infective schistosomes. We then highlight the importance of adopting a One Health approach to eliminate schistosomiasis and discuss potential interventions targeting livestock in SSA that could facilitate progress towards elimination. Finally, we discuss the challenges and next steps associated with implementation of a One Health strategy.